Diabetic Retinopathy
Jump to: Symptoms | Diagnosis | Treatments | Research and Health Policy | Clinical Trials | Resources
Overview
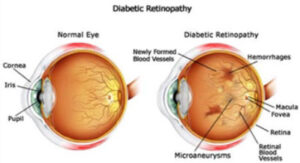
Diabetic retinopathy (DR) is the most common form of vision loss associated with diabetes. Affecting approximately 1 million Canadians, it is the leading cause of blindness among working-age adults. When left untreated the condition may advance into diabetic macular edema (DME), where damaged blood vessels leak into the macula, the central area of the retina, resulting in blurred vision and dark or distorted images. If you have diabetes it is important to have regular appointments with your eye specialist to undergo specialized screenings, which will test to see if your eyes are showing signs of retinopathy. Since the early stages of the disease do not always carry symptoms, these screenings are essential; there is no reliable cure for vision loss resulting from diabetic retinopathy, but the disease can be managed—and vision loss prevented—if it is diagnosed early enough before damage to the retina occurs.
In the “non-proliferative” form of diabetic retinopathy, blood sugar levels from diabetes damage the blood vessels that nourish the retina, the light-sensitive tissue at the back of the eye. This damage will often lead to dot-like hemorrhages throughout the retina. These often don’t carry any symptoms, however, and with adequate control of diabetes, the damage in the eye can be reversed.
Advancement of the disease can lead to fluid leaking into the retina, resulting in swelling. At this stage, which is typically diabetic macular edema, symptoms such as blurring may begin to manifest; alternatively, the patient’s vision may be normal, which is why regular eye tests are so important.
When the disease advances, new blood vessels grow to compensate for the damaged old ones, but they are weaker and more susceptible to breaking and rupturing. This is the “proliferative” stage of the disease. This can lead to bleeding into the vitreous cavity, which may present as floaters or spots in one’s vision.
The chances of developing diabetic retinopathy increase the longer you have diabetes. The disease can also increase your chances of developing neovascular glaucoma and cataracts.
Symptoms
Most people with diabetes do not realize they have developed diabetic changes in their retina. Even if you have severe diabetic retinopathy, you may not notice any vision changes. If you do notice a change, these symptoms may include:
Image distortion (straight lines appear wavy)
Blurry vision in the center
Red floaters
Sudden loss of vision
Damage to the eye may occur before diabetes is diagnosed. If you have or are at risk for developing diabetes, you should schedule regular eye exams. Speak with your eye doctor or have your health care provider refer you to an eye doctor.
Diagnosis
Early-stage diabetic retinopathy may be reversible with better diabetes control alone.
The dilated eye exam is the most common, safe, and effective diabetes eye exam. This exam involves the following:
- Drops are put into your eyes to dilate your pupils.
- Once the pupils are enlarged, the eye doctor examines your eyes using a magnifying lens that provides a view of the back of the eye.
- Your doctor examines the retina and blood vessels at the back of the eye to look for damage in your eye from diabetes.
If this exam is performed by an optometrist, it may be covered by your provincial or territorial health insurance. Ask your optometrist for more details.
If the exam is performed by an ophthalmologist, the exam is covered by provincial health insurance.
Diabetic macular edema
Advanced diabetic retinopathy can lead to diabetic macular edema (DME). DME If caught early, treatments with anti-VEGF injections or laser can be successful in reducing swelling and preventing vision loss.
Regular screenings with an eye doctor can help detect diabetic retinopathy and macular edema when it is at an early stage.
Existing Treatments
If you have diabetes it is important to:
- Monitor your blood sugar levels often
- Maintain a balanced diet that is monitored by your doctor or registered dietitian, and
- Take all medication prescribed to you by your doctor. If you are having side effects and want to stop taking your medication, tell your doctor.
Your risk of developing diabetic retinopathy increases if you do not manage your diabetes. There is no guaranteed treatment that restores vision. However, there are several treatments for slowing vision loss if you have diabetic retinopathy or macular edema.
Anti-VEGF Treatment:
Vascular endothelial growth factor (VEGF) is produced in the body and encourages new blood vessels to form. In diabetic retinopathy, the amount of VEGF increases and leads to uncontrolled growth of blood vessels in the eye. Anti-VEGF treatments block VEGF from working and can prevent and, in some cases, reverse vision loss. These treatments are delivered by an injection into the eye. They are usually the first treatment option for advanced diabetic retinopathy.
There are different types of anti-VEGF drugs, including:
- Aflibercept (Eylea®)
- Bevacizumab (Avastin®)
- Brolucizumab (Beovu®)
- Faricimab (Vabysmo®)
- Ranibizumab (Lucentis®)
- Biosimilar for ranibizumab (Byooviz®)
While all these medications reduce blood vessel growth, they all work slightly differently and may have different injection frequencies and side effects. Some of these drugs may not be funded by your provincial health plan. You should discuss with your doctor to find out which treatments are right for you.
Steroid treatment
Injectable steroids are sometimes used if anti-VEGF drugs do not work completely or stop working One example of a steroid treatment is an implant of dexamethasone (Ozurdex®) which is injected into the eye and slowly releases medication. Steroid treatment can increase your risk of developing Depending on your province, steroids may not be covered by public health insurance.
Laser surgery
Laser surgery may be used in some cases to prevent further vision loss. During surgery, your eye surgeon will shine a laser beam on the abnormal blood vessels which can help close the leaky vessels. This can reduce swelling in the retina.
Vitrectomy surgery
This procedure involves making small cuts in your eye and removing the vitreous gel and blood from the center of your eye. Scar tissue may also be removed, and a laser may be applied to the peripheral retina. The vitreous is no longer necessary and is replaced with saline solution.
Research Developments and Health Policy
Fighting Blindness Canada is committed to advancing the most promising sight-saving research, and has invested over $40 million into cutting-edge science and education since the organization was founded. Recognizing that science is tied to policy frameworks, FBC is also actively involved in health policy activities across Canada. Below is a list of some recent developments in research and policy related to diabetic retinopathy:
- Retinal imaging and detection: detecting and diagnosing diabetic retinopathy is incredibly important—the earlier the disease is found, the better the chance to prevent any loss of vision. There are several forms of imaging being used today, including OCT, OCT angiography, widefield imaging, and fluorescein angiography. Exciting developments are taking place in the field of diagnostic imaging that could facilitate rapid and early detection, including the deployment of complex algorithms capable of screening images of eyes (called “fundus photographs”). Already this software is showing an ability to distinguish images of healthy eyes from ones showing early signs of diabetic retinopathy—you can read more about some of these developments by clicking the button below.
READ MORE ABOUT THESE DEVELOPMENTS
Clinical Trials
Clinical trials are essential to the scientific process of developing new treatments: they test the viability and safety of experimental drugs and techniques, called “interventions,” on human beings. While there is no guarantee that enrolling in a clinical trial will provide any medical benefit, some patients do experience positive results after receiving experimental therapy.
READ OUR CLINICAL TRIALS GUIDE
The website clinicaltrials.gov is a centralized database of clinical trials that are offered globally. But as the disclaimer on the site’s home page states, there is no guarantee that a listed trial has been evaluated or approved—the National Institutes of Health runs the site but does not vet its content. This means that there could be bogus or dangerous trials listed that are preying on patients. It is essential that you discuss a clinical trial with your ophthalmologist before enrolling, and that you pay close attention to enrollment criteria.
If you are interested in exploring what is available on the site you can click on the button below, which will take you to clinicaltrials.gov and initiate a search for trials relevant for patients living with diabetic retinopathy.
CLINICAL TRIALS FOR DIABETIC RETINOPATHY
resources
Fighting Blindness Canada has developed additional resources that can be helpful in plotting an optimal path through vision care. Below is a link to our must-read resources, where you will find information on genetic testing, clinical trials, stem cell research, and more as well as a link to View Point (FBC’s virtual educational events).
VIEW POINT: VIRTUAL EDUCATIONAL SERIES
Health Information Line
Do you have questions about your eye health or information shared on this page? Our Health Information Line is here to support you. For resources on how to monitor your risk to prevent sight loss, check out the following resources:
- Diabetes and Vision Loss Tip Sheet ENGLISH | EN FRANÇAIS | MANDARIN 普通话 | PUNJABI ਪੰਜਾਬੀ | URDU اردو
The below video provides a basic summary of diabetic retinopathy:
Tell us what it’s like to live with diabetic retinopathy.
Share your experience by filling out our survey using the button below.
Updated on October 27, 2020.
Join the Fight!
Learn how your support is helping to bring a future without blindness into focus! Be the first to learn about the latest breakthroughs in vision research and events in your community by subscribing to our e-newsletter that lands in inboxes the beginning of each month.

