Age-Related Macular Degeneration
Jump to: How AMD Affects the Retina | Risk Factors and Causes | Dry AMD | Geographic Atrophy | Wet AMD | Research Developments | Resources | References
Overview
Age-related macular degeneration (AMD) is the leading cause of vision loss in people over the age of 55, affecting approximately 2.5 million Canadians. In AMD, central vision is affected, making it harder to do activities like reading, driving, and distinguishing faces. There are two kinds of AMD: dry AMD and wet AMD. Geographic atrophy is an advanced form of dry AMD.
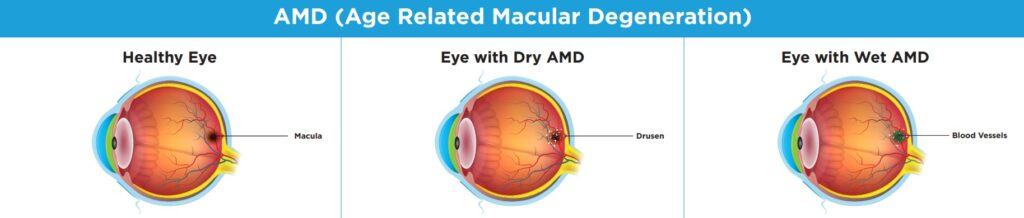
Healthy eye: The macula is a small section of the retina located at the back of the eye. The macula contains a high concentration of photoreceptor cells and is responsible for central and detailed vision.
Eye with Dry AMD: As you age, your macula gets thinner. Sometimes fat deposits, called drusen, build up and can damage the macula, causing vision loss.
Eye with Wet AMD: As the macula thins, blood vessels under the macula may start to swell and grow more than normal. These vessels can break and leak blood into the eye causing vision loss.
How AMD Affects the Retina
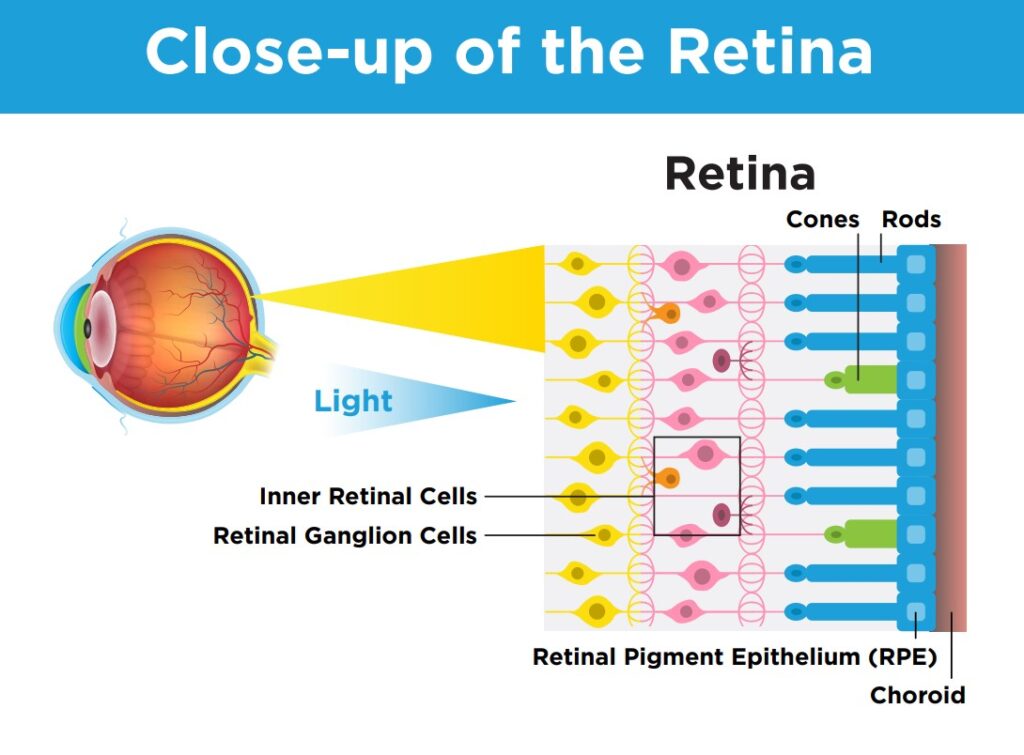
The retina is the light-sensitive tissue at the back of the eye that makes sight possible. It is composed of many cell types that work together to send a visual signal to the brain. When light hits the retina, photoreceptor cells create an electrical signal that moves through the layers of retina and travels up the optic nerve to the brain. The layer under the photoreceptors is called the retinal pigment epithelium (RPE), and these cells are responsible for providing nourishment and maintenance to the photoreceptors.
In AMD, photoreceptor and RPE cells are damaged leading to vision loss. AMD primarily causes damage to cells in the macula, which is the small, central portion of the retina responsible for detailed, central vision.
Risk Factors and Causes
The largest risk factor for AMD is age, and the disease is most common over the age of 60. Other risk factors include smoking, diet, genetics and family history of the disease and race, with AMD being more common among Caucasians. While the disease is most commonly associated with ageing, some forms, often called “macular degeneration”, can affect younger people and are caused by genetic, environmental, nutritional, and other factors.
Dry AMD
The dry form of AMD is more common and usually less severe than wet AMD. It occurs when the macula region of the retina becomes thinner. AMD is a progressive disease, meaning that symptoms normally get worse over time. Dry AMD can be divided into three stages: early, intermediate and late. In approximately 10% of individuals, dry AMD can turn into wet AMD, which causes faster vision loss. It is important that you monitor any changes in your vision and talk to your eye doctor if you experience any changes or new symptoms.
Symptoms and diagnosis
There are usually no symptoms in the early stages of dry AMD. As a result, regular eye tests are essential. An ophthalmologist or optometrist will look for a build-up of a yellowish deposit called drusen, which indicates the first stages of the macula’s deterioration.
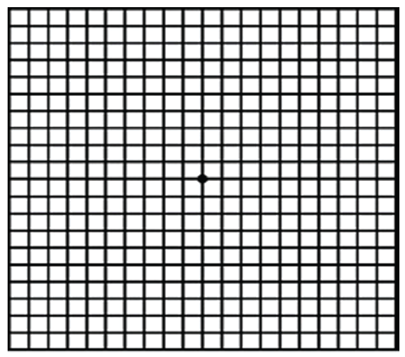
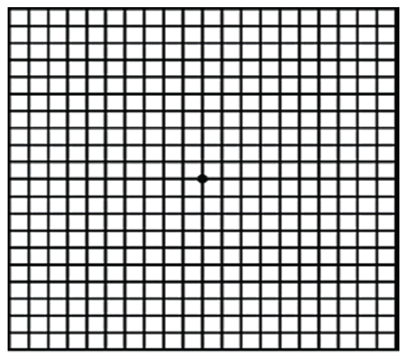
In intermediate dry AMD, you may notice a slight blurring in the field of central vision. You can detect these changes or distortions in your vision at home using a simple visual tool called an Amsler grid. This, along with other tests may be used during an eye exam.
Treatment
There are currently no treatments for dry AMD. However, if you have early-stage dry AMD, here are some things you can do that may help to reduce the risk of it progressing:
- Monitor any changes in your vision. If you notice any changes, report them to your eye doctor immediately.
- Eat a variety of foods, including fish and colourful vegetables. A healthy lifestyle with a balanced diet may help slow or prevent dry AMD from advancing into later stages.
- Get regular exercise. Many activities that protect your heart health may also protect your vision health. Speak with your doctor before starting any new exercise program.
- Quit smoking. Smoking increases your risk of developing AMD and of the disease progressing.
Because dry AMD does not affect peripheral vision it typically does not cause total blindness. The reduction of central vision can make task such as reading difficult. Low vision rehabilitation specialists can suggest techniques and technology that can help maximize a person’s remaining vision.
AREDS and AREDS2 Nutrition Supplements
Studies show that if you have intermediate or late-stage AMD, nutrition supplements may slow disease progression. One study showed that AREDS lowered the chance of dry-AMD progressing to wet AMD by 25%. [1]
AREDS2 is a newer supplement that was originally developed for smokers. In AREDS2, one of the ingredients, beta-carotene, which increases the risk of lung cancer in people who smoke, was replaced by lutein and zeaxanthin. A study published in 2022 showed that AREDS2 not only reduces the risk for lung cancer, but was also more effective in reducing the progression of AMD as compared to the original AREDS formula. [2]
AREDS and AREDS2 supplements do not restore vision that has already been lost. If you have intermediate AMD, AREDS may delay the onset of late AMD. If you have late AMD in only one eye, AREDS may slow AMD progression in your other eye. These supplements do not appear to help people with early AMD [3].
These supplements are available without a prescription, but you should consult with an ophthalmologist or family doctor before starting any new supplements.
Geographic atrophy (GA)
Geographic atrophy (GA) is an advanced form of dry AMD that affects more than 5 million people worldwide. In GA, cells in the retina start to die, creating areas of death or atrophy which cause vision loss. GA often begins near the centre of the macula, causing blind spots in the central field of vision. Symptoms can include distortions in vision, the need for brighter light when reading, difficulty adjusting to dim lights, difficulty recognizing faces and decreased brightness of colours and blurriness when reading or performing detailed tasks.
These symptoms develop slowly overtime and are not painful, meaning you may not be aware that it is happening. This is why getting a regular check-up with your eye doctor is so important. Your doctor can diagnose GA with an eye exam or retinal imaging. GA is a progressive disease and can lead to permanent vision loss.
The cause of GA is not clearly understood, but it is thought to be caused by a combination of factors that include damage from ageing, environmental factors, and genetics. If you have GA in one eye, it is more likely that you will develop it in your other eye.
There are currently no approved treatments in Canada for GA, but there are several potential treatments being tested in clinical trials. These include drugs and cell replacement therapy. You can learn more about these innovative treatments on our Clinical Trials page. Increased lighting, magnification or other low vision devices can help maximize your vision.
Wet AMD
The wet form of AMD is less common but more severe than dry AMD. Approximately one in ten people with dry AMD develop wet AMD, also called neovascular AMD. In wet AMD, blood vessels grow abnormally below the thinning macula. If left untreated, they can leak blood and fluid into the eye. This causes damage the RPE cells and can cause significant vision loss, particularly to central and detail vision. AMD does not impact peripheral vision, so it is rare for it to cause blindness.
Symptoms and Diagnosis
There is some evidence that increasing age, family history of AMD, low levels of exercise and smoking can increase the risk of progressing to wet AMD [5]. Symptoms for wet AMD can appear suddenly and get worse quickly. Symptoms for wet AMD can include:
- Vision distortion (straight lines appear bent or wavy)
- Blurring of central vision
- Dark spots or blind spots
- Difficulty seeing detail in low light
- Sensitivity to bright light
If you have been diagnosed with wet AMD, you are strongly encouraged to use an Amsler grid to monitor your vision at home. If you notice any distortions or changes in your vision, you should see your doctor right away.
Treatment
There are different treatments that can help slow progression of wet AMD, prevent further vision loss and, if started early enough, even restore some lost vision.
Anti-VEGF drugs
Vascular endothelial growth factor (VEGF) is produced in the body and encourages new blood vessels to form. In wet AMD, the amount of VEGF increases and leads to uncontrolled growth of blood vessels in the eye. Anti-VEGF treatments block VEGF from working and can prevent and, in some cases, reverse vision loss. These treatments are delivered by an injection into the eye. They are usually the first treatment option for wet AMD.
There are different types of anti-VEGF drugs, including:
- Aflibercept (Eylea®)
- Bevacizumab (Avastin®)
- Brolucizumab (Beovu®)
- Faricimab (Vabysmo®)
- Ranibizumab (Lucentis®)
- Biosimilars for ranibizumab (Byooviz® & Ranopto®)
While all these medications reduce blood vessel growth, they all work slightly differently and may have different injection frequencies and side effects. Some of these drugs may not be funded by your provincial health plan. You should discuss with your doctor to find out which treatments are right for you.
Photodynamic Therapy
During photodynamic therapy, a drug called verteporfin (Visudyne®) is injected into your arm and travels to your eye’s blood vessels. A laser then activates Visudyne, and together this can reduce blood vessels leaking. This form of combined drug and laser therapy is sometimes used with anti-VEGF treatments for specific types of wet AMD.
Laser Surgery
Laser surgery is a treatment for wet AMD that has not responded to any other treatments. The doctor uses a laser to seal abnormal blood vessels at the back of the eye and stop them from leaking. This type of laser surgery may help slow down vision loss but does not restore vision. Laser surgery causes scarring, can create blind spots and is only used in unique cases.
Research Developments
Many research groups are working to develop new treatments and cures for AMD. This includes treatments to reduce the symptoms causing vision loss, stop photoreceptor cell death, and even restore vision when it has already been lost. [6]
Some of the most promising and exciting areas of research are:
- Different pharmaceuticals, including anti-inflammatory drugs, complement inhibitors, mitochondrial enhancers, and neuroprotective agents, are being tested.
- Looking for ways to improve the outcomes of anti-VEGF treatment or improve the patient experience by developing treatments that reduce the frequency of injections. One example is a refillable reservoir that stores anti-VEGF drugs that is implanted under the eyelid and refilled infrequently using a special needle. [7]
- Gene therapies are being tested in clinical trials as potential treatments for both dry and wet AMD. Scientists are studying if gene therapy can be used to prevent photoreceptor cell death, deliver a permanent source of anti-VEGF, or reduce progression from dry to wet AMD.
- Stem cell therapies to replace retinal cells that are damaged or lost in advanced dry AMD are being tested in clinical trials.
- Retinal prostheses use technology to simulate vision. Research is underway to test if retinal prostheses may help people living with AMD.
Resources
Do you have questions about your eye health or information shared on this page? Our Health Information Line is here to support you. You can also contact us if you would like us to mail you a free Amsler grid, or download the Amsler grid here.
You can also download our AMD Tip Sheet here.
For further information about AMD and innovative treatments please visit the following resources:
The video below provides a basic summary of wet AMD:
Tell Us What it’s Like to Live with AMD
Share your experience by filling out our survey using the button below.
References
- [1] https://nei.nih.gov/health/maculardegen/armd_facts
- [2] https://www.ophthalmologytimes.com/view/nih-study-confirms-benefit-of-supplements-for-slowing-age-related-macular-degeneration
- [3] https://nei.nih.gov/health/maculardegen/armd_facts
- [4] http://www.cos-sco.ca/vision-health-information/conditions-disorders-treatments/retinal-diseases/amd/
- [5] https://www.ncbi.nlm.nih.gov/books/NBK536467
- [6] https://bjo.bmj.com/content/106/3/297
- [7] https://www.aao.org/eye-health/tips-prevention/promising-new-treatments-amd
Updated on July 21, 2023
Join the Fight!
Learn how your support is helping to bring a future without blindness into focus! Be the first to learn about the latest breakthroughs in vision research and events in your community by subscribing to our e-newsletter that lands in inboxes the beginning of each month.

